McGill researchers create model to predict chronic pain
 (Pexels)
(Pexels)
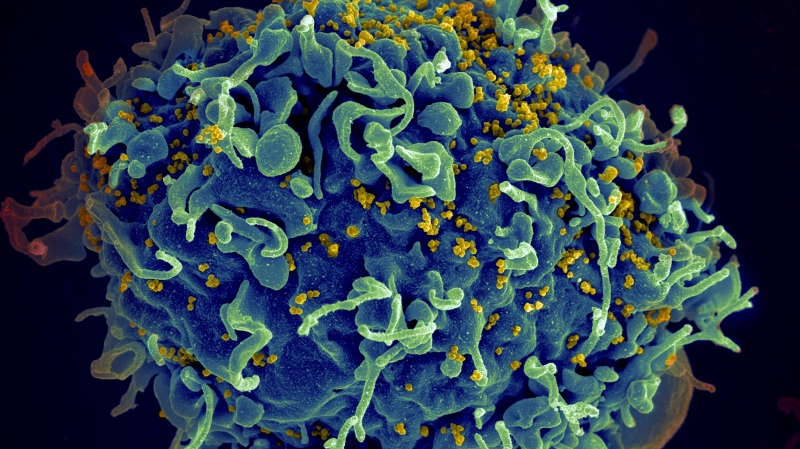
Researchers at McGill University have designed a model to predict the development of chronic pain in patients, which could be used to manage waiting lists in pain management clinics.
Published in Nature Medicine in early July, the study looked at overlapping chronic pain, i.e. when someone reports chronic pain in more than one part of their body.
Researchers used data from the U.K. Biobank, which documents health data from 500,000 people.
"The advantage of this is that, for the first time, we have access to half a million people who filled in different questionnaires, did batteries of tests, and reported the different types of pain that affected them," explains Dr. Etienne Vachon-Presseau, assistant professor at McGill's dental medicine faculty and study co-author.
Data was collected from U.K. citizens aged 50 to 70, whom the biobank follows as they age.
"We observed that many patients had chronic pain, about 40 per cent of those who took part in the study. Then, among these, there was a significant proportion, again around 40 per cent, who reported pain in several places on their body," Vachon-Presseau explained.
Thanks to this data, "we developed a predictive model, using machine learning, on a panoply of environment, psychological and personality factors -- sleep disorders, alcohol consumption, smoking, anthropometric measurements such as body mass index, for example," he said.
The researchers entered around 100 variables into the model to determine which combinations of factors can be used to predict the number of sites on the body where a person will suffer chronic pain.
"We were able to predict over time, for example, if a patient has chronic knee pain -- is that patient at risk over time of having their pain develop at other sites? For example, we start with the knee, but end up with four more sites, nine years later -- back pain, hip pain, neck pain, shoulder pain," Vachon-Presseau illustrated.
Although the model is most effective when analyzing the development of chronic pain in a person who already suffers from it, under certain conditions, it can predict whether someone who doesn't experience chronic pain at present will suffer from it later.
But the "performance was a little lower" in this latter application, Vachon-Presseau notes.
A TOOL TO MANAGE WAITLISTS?
Asking 100 questions to predict the evolution of a patient's chronic pain isn't realistic, "so we sacrificed a bit of the model's performance" and reduced it to six main factors, said Vachon-Presseau.
These factors are sleep, neuroticism, fatigue, recent consultation with a doctor for mental health issues, life stressors (such as death, divorce, and financial difficulties), and body mass index.
"We'd like to implement the model in pain clinics, to see how it really performs with patients in tertiary care units."
It could be used, "for example," in the evaluation, the screening of patients, to know whether they should be prioritized because they are more at risk, or in the opposite case, whether the person can perhaps wait a little longer on the waiting list."
Vachon-Presseau pointed out that wait times can be over a year for some patients.
If the model "performs well," it could also prompt clinicians to prescribe more aggressive treatments if a person is at particular risk of their pain spreading.
The model could also be used for research purposes, Vachon-Presseau added.
This report by The Canadian Press was first published in French on Aug. 5, 2023.
CTVNews.ca Top Stories

Canadian team told Trump's tariffs unavoidable right now, but solutions on the table in surprise Mar-a-Lago meeting
During a surprise dinner at Mar-a-Lago, representatives of the federal government were told U.S. tariffs from the incoming Donald Trump administration cannot be avoided in the immediate term, two government sources tell CTV News.
Pedestrian killed by Via Rail train near Kingston, Ont.
Regular rail traffic has resumed with severe delays.
Muskoka reacts to major snowfall, hundreds stuck on Highway 11
From road closures, power outages, weather declarations and nonstop shovelling, Muskoka residents were faced with nearly a metre of persistent snowfall on Saturday.
Saskatoon priest accused of sexual assault says he meant to encourage young girl with hug and kiss
A Saskatoon priest accused of sexual assault says he meant to encourage and reassure a young girl when he hugged and kissed during his testimony at Saskatoon Provincial Court Friday.
Trump threatens 100% tariff on the BRIC bloc of nations if they act to undermine U.S. dollar
U.S. president-elect Donald Trump on Saturday threatened 100 per cent tariffs against a bloc of nine nations if they act to undermine the U.S. dollar.
Toronto man accused of posing as surgeon, giving four women injections
A 29-year-old Toronto man has been charged after allegedly posing as a surgeon and providing cosmetic procedures on several women.
Bob Bryar, drummer for rock band My Chemical Romance, dead at 44
Bob Bryar, former drummer for the band My Chemical Romance, has died. He was reportedly 44.
'Disappointing': Toronto speed camera cut down less than 24 hours after being reinstalled
A Toronto speed camera notorious for issuing tens of thousands of tickets to drivers has been cut down again less than 24 hours after it was reinstalled.
W5 Investigates 'I never took part in beheadings': Canadian ISIS sniper has warning about future of terror group
An admitted Canadian ISIS sniper held in one of northeast Syria’s highest-security prisons has issued a stark warning about the potential resurgence of the terror group.