The PQ leadership candidate who led the drive to create Quebec's medical dying law is coming out swinging against the MUHC.
Veronique Hivon said the McGill University Hospital Centre is not applying the law in the spirit it was intended – but not everyone agrees.
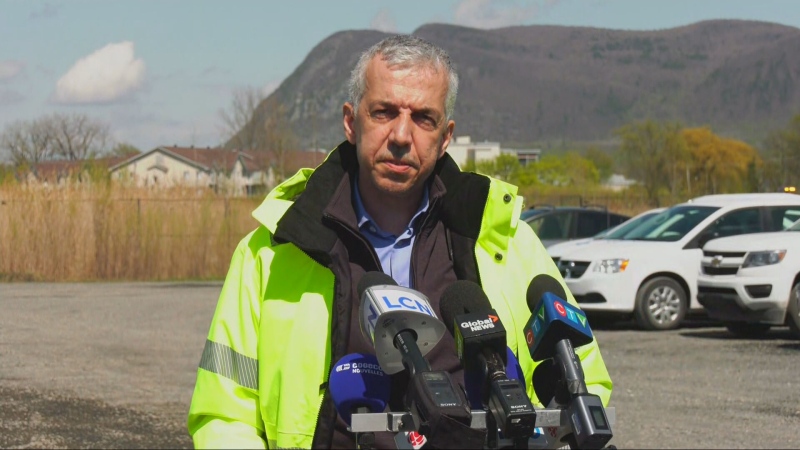
“The MUHC is offering medical aid in dying to any patient who should require it here at the hospital,” said Dr. Ewa Sidorowicz, associate director of medical affairs and professional services at the MUHC.
In mid-April, a patient at the MUHC received medical help to die.
This patient had to be moved out of the palliative care unit to another unit at the MUHC to receive the service, because the palliative care unit has a policy to not provide medically-assisted death.
“It stemmed from a concern that it may send mixed signals to patients and to families,” explained Sidorowicz.
The institution helped the patient end their life in another part of the hospital.
Neither the patient nor the patient's family ever complained, but Joliette MNA Hivon, who drafted the legislation when the PQ was in power, said it's problematic.
“It is not a policy that respects the spirit or philosophy of the end-of-life bill… because everything - the organization - has to be centred around the patient,” she said.
Quebec's College of Physicians disagreed, saying that all hospitals are going at their own speeds, and that the MUHC's policy is part of normal adaptation to a new law that comes with serious ethical implications.
“It's not so surprising to see that. We saw it also at the palliative care unit at the CHUM, as a matter of fact,” said Dr. Yves Robert, head of the Quebec College of Physicians. “We saw the reverse also, where other units didn't want to provide the service and asked the palliative care unit.”
Robert said the legislation is clear.
“They can have their own politics to offer the procedure in any other units or area of the MUHC and they will fill out the requirements of the law,” he said.
The law says that every patient can end their life in a hospital, hospice, or their home, but does not say that all units in a hospital must allow doctors to end a person's life.
Hivon said that that is not her preferred approach.
“You're right, but I find it very disturbing that in a policy it is stated, black on white on Section 3 that it can be provided in the institution, but specifically not in the palliative care unit,” said Hivon.
That is likely to change, said the MUHC’s Sidorowicz, as a result of a discussion that started back in mid-April, well before this story was made public.
“As this case has been reviewed, it has triggered a lot of questions with our palliative care group, actually, and my suspicions are that in the next little while there will be an evolution of the policy to include the palliative care unit,” she explained.