MONTREAL -- The days in the emergency room at St-Mary's Hospital in Montreal don’t drag on or fly by.
“No, they all blur together,” said nurse Beatrice Roumeliotis.
“It’s really like Groundhog Day, every day you wake up, and I’m like ‘Okay, am I working?'” said Lea Anne Hogan, another nurse on the frontlines at St-Mary’s.
It’s been eight weeks since the COVID-19 pandemic has taken hold of the city, and Montreal ERs are feeling the pressure – nurses are working under extraordinary conditions at their own personal risk.
Hogan, who’s been a nurse for 24 years, said working amid the pandemic has been dominated by two themes: constant change and intense stress.
“We’re experiencing things that I don’t even think I’ve even dreamt of before. It’s every day that we’re exhausted mentally, physically,” she said.
At St-Mary’s, a garage that usually houses ambulances has been transformed to accommodate COVID-19 patients through a new triage system to minimize the risk of transmission.
“If you have any of those symptoms you’re going to go directly to the triage in the garage,” Hogan said. “The garage triage is a yellow zone, so a potential.”
When CTV News visited the hospital on Tuesday – International Nurses’ Day – an elderly man with a fever showed up for a test. Another man whose wife tested positive for COVID-19 did, too.
Inside the ER, there’s a green zone for patients who raise no COVID-19 flags, and a hot zone for ones who need more care. But the environment isn’t the only thing that has changed drastically since the start of the pandemic.
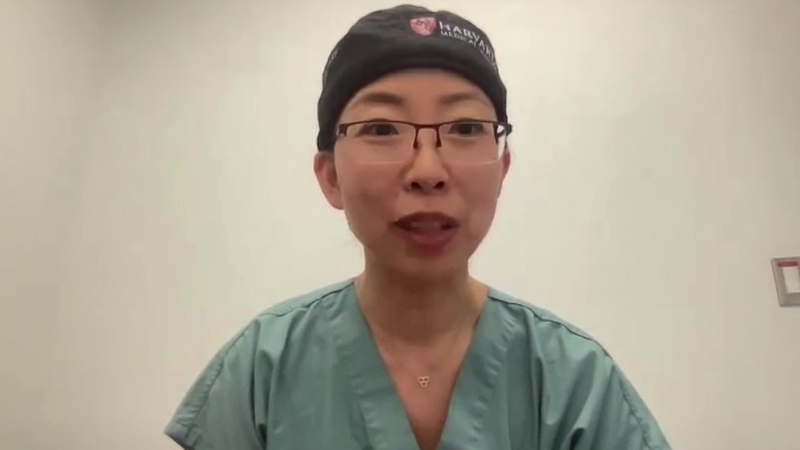
“It’s been huge, we’ve had to rethink every process from the time a patient enters to the time a patient leaves,” said Dr. Suj Sivaraman, the chief of emergency medicine at St-Mary’s.
The changes have been difficult for nurses who are used to putting their patients first.
“We would rush to a patient in the past,” Hogan said. “Now all of a sudden we have to stop, get gowned up, make sure we’re all protected, and then you can go in. So that’s a very different mentality for a nurse to try to come to grips with.”
Roumeliotis echoed her colleague’s feelings.
“It gets really heavy when you have geriatric patients who are completely delirious, their veins are terrible, their veins are blowing, they’re unstable, they’re trying to climb out of bed but they’re gasping for air,” she said. “It’s emotionally draining as well because you wish you could be there next to them the whole time, but we can’t be doing that right now.”
In normal times, heading home from work after a difficult shift might be a breath of fresh air – but not for front-line workers who have to isolate from their loved ones to keep them safe.
“My wife and I realized very quickly that the biggest threat to my family was me,” Sivaraman said. “I haven’t hugged my kids in two months.”
Hogan, who has teenage children, wasn't able to see them on Mother's Day, and isn't sure when it will be safe to be around them again.
“That was the hardest, I think,” she said. “I’m extremely close to my children and it was like ‘Wow, how long is this going to go on for?’ ”
Despite the difficult working conditions, staff at St-Mary’s say they can lean on each other when they need to.
“You go home, you cry, you talk to your fellow colleagues. You have to let yourself feel,” Roumeliotis said. “If we don’t feel empathy, then we’re not nurses.”