Joanne Derose is starting her last week of chemotherapy treatment for uterine cancer, and it’s been ravaging her body.
“I feel like a rag doll, like you have Jello legs, just going up six steps, I'm out of breath,” she said.
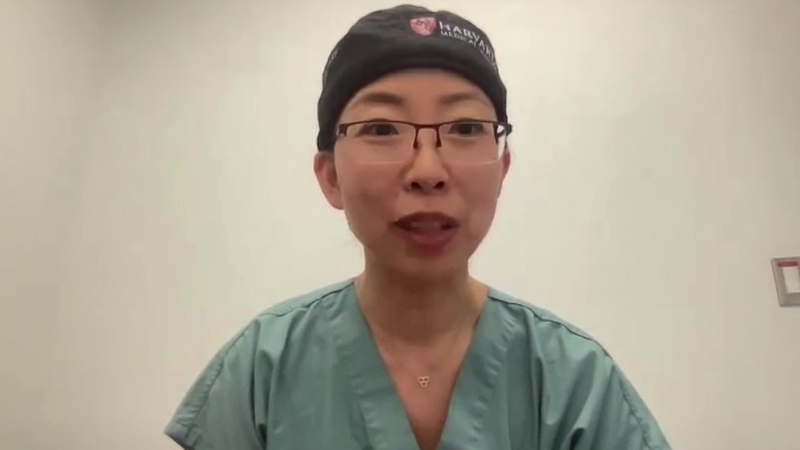
Dr. Lucy Gilbert,the director of gynecologic oncology at MUHC, says standard chemotherapy doesn’t differentiate between cells. She describes it as a blunt tool – it kills cells whether they’re cancerous of not.
“[It’s] a sledgehammer - it hits all the cells that are multiplying, it hits the bone marrow, it hits the lining of our gut, it hits nerves,” she said.
The same type of chemotherapy is used to treat ovarian cancer, and while some patients are cured, if the ovarian cancer recurs it’s incurable.
Health Canada is expected to approve a new drug for women with ovarian cancer soon. Called “PARP inhibitors,” it is already available in the U.S.
“They are targeted therapy … it harms the cancer cells far more than it harms the good cells,” said Dr. Gilbert.
Daniela Serindac was diagnosed with ovarian cancer in 2011. She says the first round of chemo was punishing.
“It's hard time for the body, it's hard time for the mind,” she said.
A year and a half later the cancer returned. That round, she describes as “terrible.” Her salivation glands shut down, she had chronic pain in her fingers and little sensation in her feet. She was so exhausted she missed out on precious family time.
The PARP inhibitor pills are prescribed after chemo as a kind of maintenance drug. The side effects are mild.
Dr. Gilbert is heading up a research protocol on the drug at the MUHC and Dr. Diane Provencher is doing the same at the CHUM.
“It's certainly exciting, it's in the line of doing personalized treatment also, it's not applicable to everybody,” she said.
So far, the drug is given to patients with a gene mutation, about 100 women a year.
Studies show that when their cancer recurs, the PARP inhibitor can more than double the time between chemo treatments, going from 4 months to 11 months cancer free. And most importantly, they have better quality of life before the cancer comes back.
Serindac is taking part in the study. She says she hasn’t experienced any side effects and feels well.
Doctors hope all eligible patients will soon have access, but there's a hitch. Since the drug is new and data is limited, Health Canada will likely follow the lead of the American FDA,and direct doctors to prescribe it only after the third or fourth round of chemo. Doctors here say that's too late.
“I say don't wait for overall survival data. Give people good quality life at the time they can enjoy it, their family can enjoy it,” Dr. Gilbert said.
If the doctors prescribe it the way they want to and ignore Health Canada’s guidelines, the patient will have to pay for the drug herself. Right now it costs about $12,000 U.S. a month.
Doctors have written to Health Canada voicing their concerns, but Health Canada would not confirm whether they take into account the appeals of outside experts.
“And I think as physicians and patients, we have to demonstrate to the government that quality of life, even if it's not that long, it means a lot,” Provencher said.
Serindac says the new treatment has made all the difference, giving her limited, but quality time. She wants others to have the same chance.
“If you have no choice you try everything to have one more day, but when there is a choice I think the people have to think again because it's a hard life when you have chemo many times,” she said.