TORONTO -- The death of a Quebec mayor who was stung multiple times after stepping on a wasps' nest while gardening is a tragic but cautionary tale for those who run afoul of bees, hornets or other stinging insects -- especially if they have a severe allergy to their venom, experts say.
Lucie F. Roussel, mayor of La Prairie, died in hospital Sunday after being stung at least 15 times in the garden of her cottage near Stratford, municipal authorities said.
There are conflicting reports as to whether the 51-year-old widowed mother of two teens had an allergic reaction, but La Prairie spokeswoman Chantal Charron said Roussel had never been diagnosed with an allergy to wasp stings.
"She was not diagnosed by a doctor. She did not know that she was allergic -- if that was the case," Charron told The Canadian Press, noting that Roussel had emergency injectable epinephrine at her home because her late husband had been allergic.
Dr. Susan Waserman, an allergist at McMaster University, said it's extremely uncommon for someone to die as a result of insect venom directly, although there are a few cases in the medical literature.
"It's possible, but it's rare," Waserman said Tuesday from Hamilton. "This is not a common phenomenon."
Most deaths that result from insect stings are caused by a severe allergic reaction known as anaphylaxis, which can be marked by such symptoms as breaking out in diffuse hives, having difficulty breathing, feeling lightheaded and sometimes vomiting, she said.
"Usually, most acute allergic reactions occur within minutes to an hour," Waserman said, noting that people may feel their tongue start tingling and their throat swelling.
"And if you have no reason to believe you are allergic, many people are caught off guard, and they don't generally carry an epinephrine auto-injector."
Symptoms of anaphylaxis can vary from one person to another and even from one reaction to the next, said Beatrice Povolo, a spokeswoman for the charitable advocacy group Anaphylaxis Canada.
What makes this allergic reaction so life-threatening is that the airways swell and close up, the blood pressure plummets and the heart starts beating irregularly -- all signs the person is experiencing anaphylactic shock.
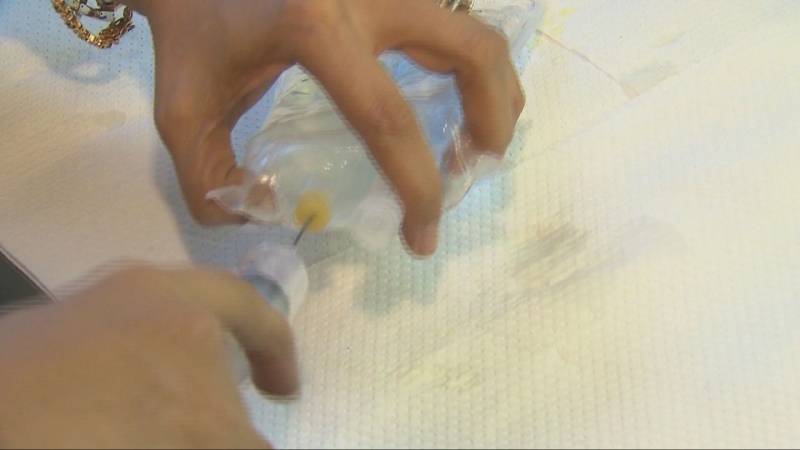
"Our key messaging to patients is always to be prepared," said Povolo, advising anyone with a diagnosed allergy to insect stings to carry two epinephrine auto-injectors, the second as backup or in case a double dose is needed.
Epinephrine is a form of adrenalin, given by a shot typically in the muscles of the thigh, that can counteract the allergic reaction until the affected person can receive medical treatment in hospital or by paramedics.
"Realize that all the EpiPen does is buy you time," stressed Dr. Mitch Shulman, a Montreal emergency medicine specialist who has treated many patients for stings over the years, including some who developed anaphylaxis.
"If you've used the EpiPen, you must be seen in an emergency room or by somebody who's competent. And the reason is the venom is still in your system," he said, explaining that the epinephrine will wear off, potentially allowing a rebound reaction hours later, which can be even more serious than the original attack.
Waserman said that sometimes people don't know they are allergic to insect venom, even though they may have already been stung once before.
"Often it takes some degree of exposure in order to become allergic, so that most people think that a first exposure isn't enough. But a lot of times, people don't remember ever having had a first exposure or they've had it but had such a mild reaction or no reaction."
Anyone who suspects they may be allergic to stinging insects should ask to be referred to an allergist, who will do skin tests to confirm if they react to the venoms of particular bugs.
If any of the tests are positive, the patient can begin immunotherapy -- a series of shots incorporating the venom that are usually given over a five-year period to gradually build up protective antibodies that prevent an allergic reaction.
There are two brands of epinephrine auto-injectors sold in Canada -- EpiPen and Allerject -- which Waserman said can be purchased without a prescription from pharmacies across Canada. Unused, EpiPen's effectiveness lasts about a year, while Allerject is good for about 18 months, she said.
Even those without a diagnosed allergy might be wise to carry one when outdoors, Waserman said.
For "people who are in the country, far from medical care in remote areas, it's not a bad idea if you're an outdoorsy person ... to keep an epinephrine auto-injector with you in the event that something like this arises out of left field," she advised, referring to Roussel's case.
"It's not common, but in adults venom is a major cause of anaphylaxis. We're not talking about huge numbers of people -- only about two per cent of Canadians are at risk. We do not have many deaths across the country -- every year, maybe three or four people in Canada at most."
Still, potentially life-threatening allergies to insect stings, foods and other substances are on the rise in Canada and elsewhere in North America, said Povolo.
While completely avoiding bugs is virtually impossible during the warm-weather months, gardens, golf courses and cottage country are particular outdoor hotspots for insects like honey bees and yellow jackets, which can deliver more than just a sting to those susceptible to allergic reactions, she said.
Her message is simple: "Really be conscious of your surroundings and always be prepared."